It’s a nice sunny day.
The kids have been playing outside in the pool for hours. After a delicious cookout, Dad is cleaning the dishes.
Suddenly, a glass slips from his hand and shatters on the floor. In his haste to prevent the tragedy, he slices his hand on a piece of glass. He tries for 30 minutes to stop the bleeding, but it’s clear… this one needs stiches!
He winces at the thought of spending hours in the Emergency Room (ER). But there’s an urgent care just minutes from his house. He heads over there, hoping for a relatively quick and painless way to get his stiches and start the healing process.
But there’s a problem.
A problem that started well before the day he cut his hand.
A problem that began with a misguided decision made by someone in the purchasing department of the urgent care.
A problem that resulted from a focus on price instead of value.
This problem is far from trivial. In fact, it will end up costing Dad – the patient – more money and extra hassle. It will also result in lost revenue for the urgent care and higher healthcare costs overall.
So how did this lose-lose scenario develop?
Below, we will examine how. And along the way, you will learn how to make sure you don’t make the same kinds of mistakes in your healthcare decision-making.
By the end of this article, you will:
- Recognize negative consequences of making decisions in healthcare based on price alone
- Build understanding of how factors beyond price can affect key healthcare stakeholders in negative ways
- Learn how to make better decisions in healthcare by examining value over price… every time
Negative consequences of making decisions based on price alone
Several months ago, the urgent care leadership was looking for ways to cut expenses.
After review, someone identified suture kits as a potential target. With an alternate supplier, the corporation would achieve estimated savings of over $1.7 million per year.
Sounds great!
But it isn’t.
The corporation’s analysis was incomplete. They didn’t consider the total cost of the switch. They stopped at price and skipped the work involved to determine value.
And it cost them…
You see, they didn’t anticipate the domino effect that followed.
Let’s take a look at what happened once the cheaper suture kits found themselves in the clinic.
Providers, having the skills to do the job soon learned that they had inadequate tools. The new (cheaper) suture kits were associated with multiple problems…
- First, as they started to suture their patients, they noticed the sutures would “tear away” from the skin. Not exactly ideal for lining up the edges of the wound for limited scarring.
- Second, the tweezers in the suture kit didn’t fully close. As a result, the providers were unable to grab the sutures well to pull them through the skin firmly.
- Third, the sutures often fell off the needle. Not only did this slow down the process, but the challenge of rethreading the needle over an open wound was frustrating.
Ultimately, the providers found the quality of the sutures was subpar… in-line with their cheaper price.
Once the realization of inadequate suture kits was well-known in the organization, the domino effect accelerated.
Providers stop suturing patients.
Instead, they referred these patients straight to the ER. And because they stopped suturing, they stopped billing for those services. Thus, an insurance charge that could be ~$500 became just a fraction at ~$150. As such, the cheaper sutures led to decreased revenue for the urgent care.
Furthermore, the patients are now at the ER, where they charge three to five times more to resolve the same medical problem. This is an example of the kind of waste that drives healthcare costs higher for everyone. The waste, however inappropriate or avoidable, still needs to be paid for. As such, health insurers raise premiums to cover these costs.
And the biggest losers of all are the patients. They waste time and money with a stop (and a charge) at the urgent care before being sent to an even more expensive site of care to get the stiches they actually need.
How to consider value instead of price alone
So what kind of analysis SHOULD have been done at the urgent care?
In short, one that looked at value instead of just price.
Recall that value includes more than price alone. It involves considering the context around that price. It involves incorporating the benefits that are gained (or lost) in exchange for any given price.
So in the case of suture kits in an urgent care setting, what context should we consider?
When we are unsure where to start, it is always helpful to go back to the basics. We want to consider a holistic view that includes #1) the use of healthcare services and products and #2) their associated costs. Some of the big categories include:
- Medical services
- Inpatient (e.g., hospital)
- Outpatient (e.g., doctor’s office)
- Emergency Department (ED)
- Urgent care
- Medical supplies
- Medications
- Laboratory tests
Our goal is to make better decisions about how to increase care quality while decreasing costs by considering which of these apply.
In the case of the urgent care, let’s consider which pieces may be impacted.
We have already described how key medical service utilization components of interest are the urgent care and the ED. Suture kits are our medical supply of interest.
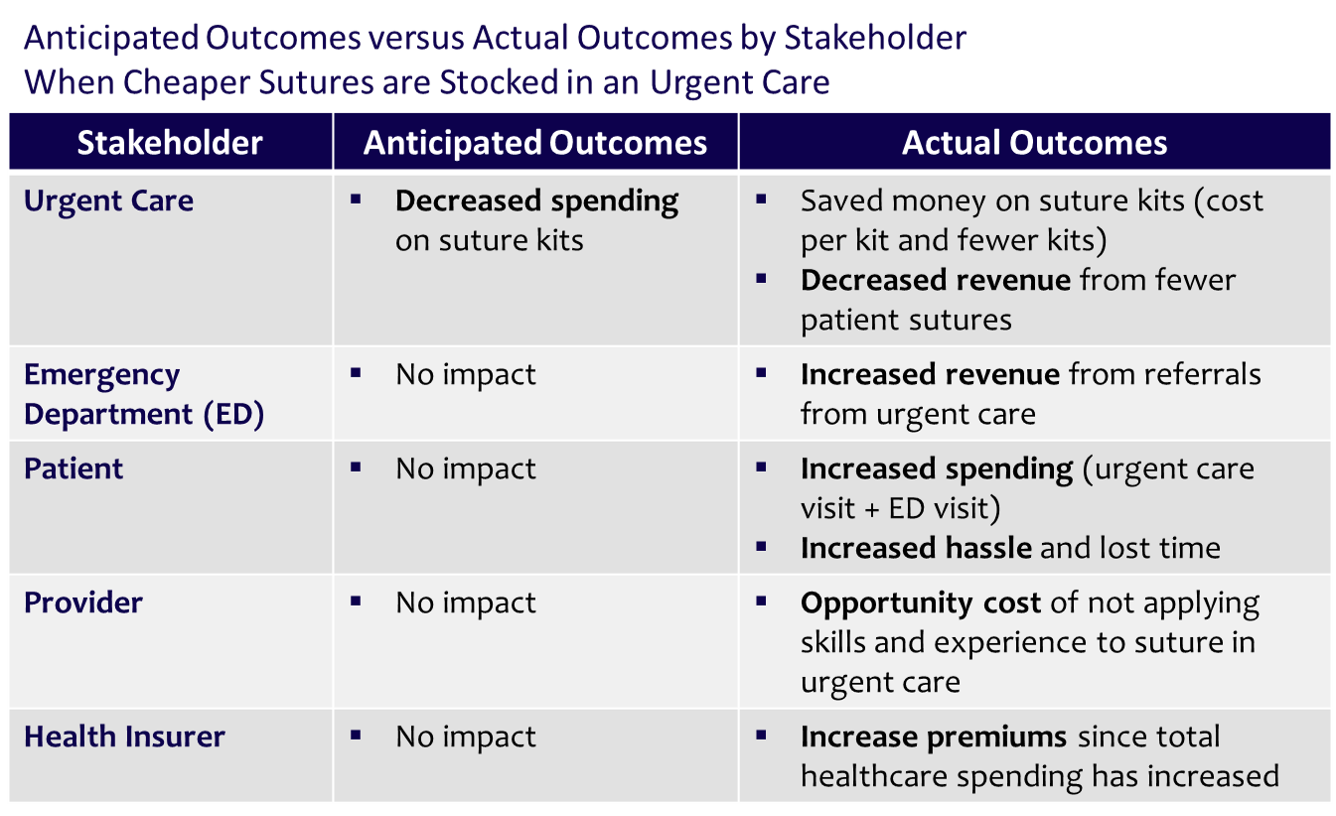
These three pieces alone are able to help us build our bigger picture about the impact of switching to cheaper suture kits. We consider that the cheaper suture affect key stakeholders in the following ways:
Urgent Care
- Reduced spending on sutures (cost per kit and fewer kits)
- Reduced revenue from loss of suture procedures performed by staff
Emergency Department (ED)
- Increased revenue from urgent care referrals
Patient
- Increased spending – urgent care visit charge plus ED visit charge
- Increased hassle and lost time from visit to two separate sites of care (urgent care and ED)
We also consider the impact on providers. There is an opportunity cost associated with the fact they are not practicing “at the top of their license” – meaning, their full skill set goes unused.
Ultimately, health insurers increase premiums to cover the waste in paying for sutures administered at the ED instead of the urgent care.
Benefits of deciding on value instead of price alone
Now let’s consider what should have happened when the urgent care considered what they were spending on sutures.
In short, they should have considered more than just what they paid for sutures. The should have also thought about what they got (Read More).
In other words, they should have taken a value approach.
So what would that look like?
First, the urgent care should have considered the impact of changing suture kits that goes beyond price. We all understand the old adage “you get what you pay for,” so it seems reasonable someone would at least consider examining the change in quality that comes with the new brand of sutures.
Second, the urgent care leadership should have thought about what they really got with the change in suture kits. If the kits were identical but at a cheaper price, they unlocked real value.
But in this case, there were notable quality differences. With proper analysis, leadership would have revealed deficiencies. They would have avoided many negative consequences for their staff (i.e., the providers), their customers (i.e., patients) and their own bottom line.
So how can we build an analysis that takes all these components into consideration?
We can do this with some simple modelling. With a model that includes a few of these elements, we can paint a clearer picture to inform decision making.
First, let’s take a look at what the urgent care leadership expected to happen. In this case, they expect to get a 20% discount on the cost of suture kits. Since they only considered price, they don’t anticipate any change to their income. Here’s what that looks like when we model it:
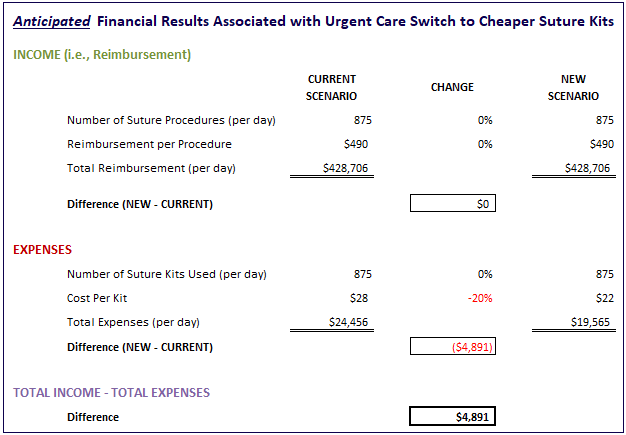
As expected, the model shows us we add just over $4,800 to our bottom line each day through the use of cheaper suture kits.
Next, let’s consider what actually happened in the urgent care when the new suture kits were deployed. Remember, while the urgent care saved money on purchasing the sutures (20% discount), they dramatically reduced the number of suture procedures performed in their clinics (~50%). Here’s what that looks like when we model it out:
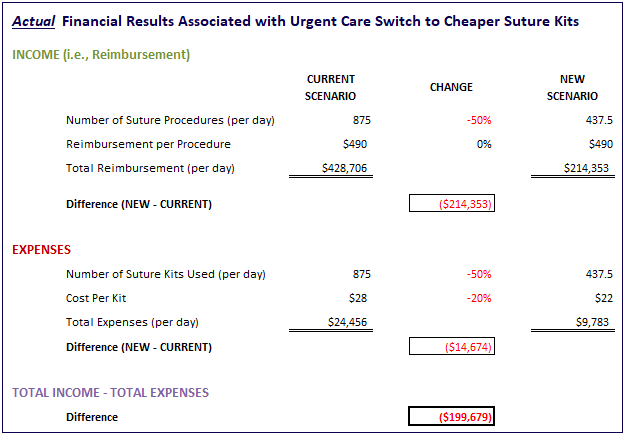
So instead of adding ~$4,800 to our bottom line each day with cheaper sutures, we are actually losing nearly $200,000 from suture procedures never performed (or billed for). This loss even includes the savings from not using as many suture kits (i.e., only 437.5 vs 875 kits).
Finally, let’s consider the fact that there may be a discount on sutures that is worth the lost revenue from its impact on the number of suture procedures performed at the urgent care. We can use our model to get an idea of just how easy or difficult it would be to do that.
Let’s start with a massive discount on sutures – i.e., 50% – and a relatively small anticipated reduction on the number of suture procedures – 5%. Here is what our model shows us:
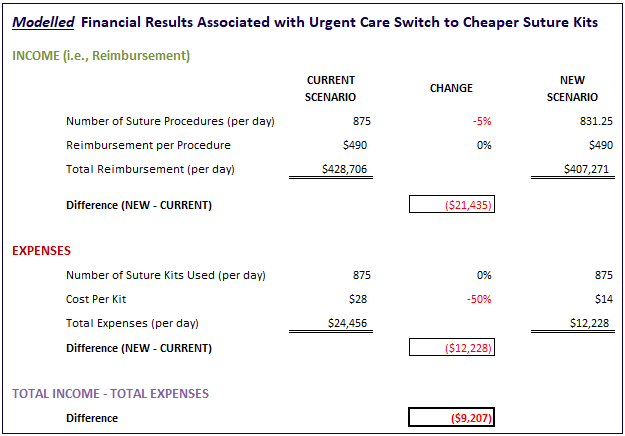
Our key conclusion with just this one scenario is that it would be very difficult to overcome any decrease in suture procedures with a product discount on suture kits. Even with a massive suture kit discount (50%) and a small impact on number of procedures (5%), the urgent care still lost over $9,200 each day!
Hopefully, you can see the value of building a simple model like this to help inform decision-making in your own healthcare environment.
Conclusion: The true cost of cheap supplies in healthcare
In this article, we have covered a cautionary tale of the consequences of making decisions in healthcare focused on price instead of value.
Specifically, we saw how cheaper sutures in an urgent care setting drove massive losses on the medical reimbursement side. These losses were mediated by a reduction in the number of suture procedures performed by the urgent care staff. These staff learned quickly that the poor quality of the cheaper sutures compromised their ability to suture well. As such, they did what was best of the patient and sent them elsewhere to close their wounds.
We are now able to:
- Recognize negative consequences of making decisions in healthcare based on price alone
- Build understanding of how factors beyond price can affect key healthcare stakeholders in negative ways
- Learn how to make better decisions in healthcare by examining value over price… every time
You can use the skills highlighted in this article to make better decisions in healthcare. When you focus on value over price, you make decisions more confidently… every time.
We hope you have found this article useful in your own value assessment efforts. If you have any questions or comments, please contact us here.
